Did you know? Nearly 20% of adults over 50 experience swollen ankles and edema at some point — often missing early signs of serious conditions such as heart failure or venous insufficiency. Swelling in your lower legs and ankles is more than an inconvenience; it’s a warning sign your body can’t afford for you to ignore. From everyday causes like fluid retention and long periods of standing, to urgent health issues like blood clots, learning what your symptoms really mean can protect your well-being. In this comprehensive guide, you’ll discover how to recognize, evaluate, and manage swollen ankles and edema — empowering you to take confident control of your leg health today.
A Surprising Truth About Swollen Ankles and Edema
"Nearly 20% of adults over 50 experience swollen ankles and edema at some point — often missing early signs of serious conditions such as heart failure or venous insufficiency."
Swollen ankles and edema aren’t just nuisances after a long day on your feet. They’re experienced by one in five adults over 50, yet many individuals fail to recognize when this swelling signals something serious. Swelling can hide underlying concerns such as venous insufficiency (where faulty vein valves interrupt blood flow) and even heart failure, which prevents your heart from pumping efficiently. Early recognition is crucial: untreated edema can lead to persistent discomfort, reduced mobility, and dangerous complications like blood clots. If you’ve ever noticed your lower legs puff up—especially if accompanied by aching, color changes, or breathing issues—understanding the true significance of swollen ankles could be life-changing.

What You'll Learn About Swollen Ankles and Edema
In this article, you'll uncover vital facts and practical tips to help you distinguish normal swelling from potentially life-threatening edema. You’ll understand the main causes, spot critical signs, and learn daily habits for prevention and relief.
- The causes and risk factors behind swollen ankles and edema
- Key differences between fluid retention, venous insufficiency, and other contributors
- How to recognize when swollen ankles signal a dangerous health issue like blood clots or heart failure
- Prevention and self-care tips
- When to consult a doctor for swollen ankles and edema
Understanding Swollen Ankles and Edema
What Is Swollen Ankles and Edema?
Swollen ankles and edema describe a condition where excess fluid accumulates in the tissues of your lower legs, ankles, and feet. This swelling, medically called oedema, often results from an imbalance in the body’s ability to regulate water, salt, and blood flow. While minor fluid retention after standing or in hot weather is common, persistent or severe swelling could point to underlying circulation or heart problems. The swollen area may feel puffy, tender, or tight, and you might notice marks in the skin where socks pressed. Recognizing early signs, such as a swollen ankle that doesn’t improve after rest, can register the need for timely medical evaluation and intervention.
It’s important to distinguish between normal swelling and edema linked to chronic health concerns. Edema may occur when you sit or stand for long periods, consume a high salt diet, or as an initial reaction to hot weather. However, if your swelling erupts suddenly, is localized to one limb, or occurs with symptoms like pain or redness, doctors advise seeking medical attention promptly. Since fluid retention in the lower legs may herald issues with the lymphatic system, heart failure, or blood clot development, never overlook changes in your ankles and feet.
The Link Between Fluid Retention and Swollen Ankles
Fluid retention is a primary driver of swollen ankles and edema. Your body’s circulatory system constantly moves fluids through your blood vessels and into surrounding tissues. If that flow is disrupted—by high blood pressure, restricted veins, lymphatic blockage, or compromised heart function—fluid can pool in the lower leg. This pooling leads to visible swelling and, sometimes, a sensation of heaviness or “fullness” in the legs and feet. Diet also plays a key role; a diet high in salt can increase water retention and exacerbate ankle swelling.
In addition to salt intake, other triggers include certain medications, standing or sitting for long periods, and specific medical conditions that affect circulation. For instance, pregnant women often notice increased swelling due to hormonal changes and fluid shifts. Whether triggered by lifestyle factors or medical issues, understanding how and why fluid collects in your legs and ankles is the first step toward effective management.
For those interested in practical strategies to address fluid retention and its impact on daily life, exploring targeted self-care routines can make a significant difference. You may find it helpful to review step-by-step guidance on daily exercises, leg elevation, and compression techniques, as outlined in our comprehensive guide to managing fluid retention and swelling.
How Fluid Retention Affects Your Legs and Feet
When fluid builds up in the lower legs and feet, it overwhelms the capacity of veins and lymphatic vessels to return fluid to the heart. The result is stretching of the soft tissues—skin, fat, and even muscle—often noticeable as puffiness around the ankles or a shiny appearance on the skin. In severe cases, this swelling can make shoes feel tighter or leave deep marks in the skin from elastic socks (an effect called pitting edema).
Chronic fluid retention can have more serious implications. Over time, persistent pressure from excess fluid may weaken skin and underlying tissue, making infections, sores, or ulcers more likely. The lymphatic system, which helps clear excess fluids, can become overwhelmed, especially if venous insufficiency or a blood clot is blocking normal flow. Recognizing these subtle, yet important, changes in your legs and feet can help you intervene before complications arise.
Common Causes of Swollen Ankles and Edema
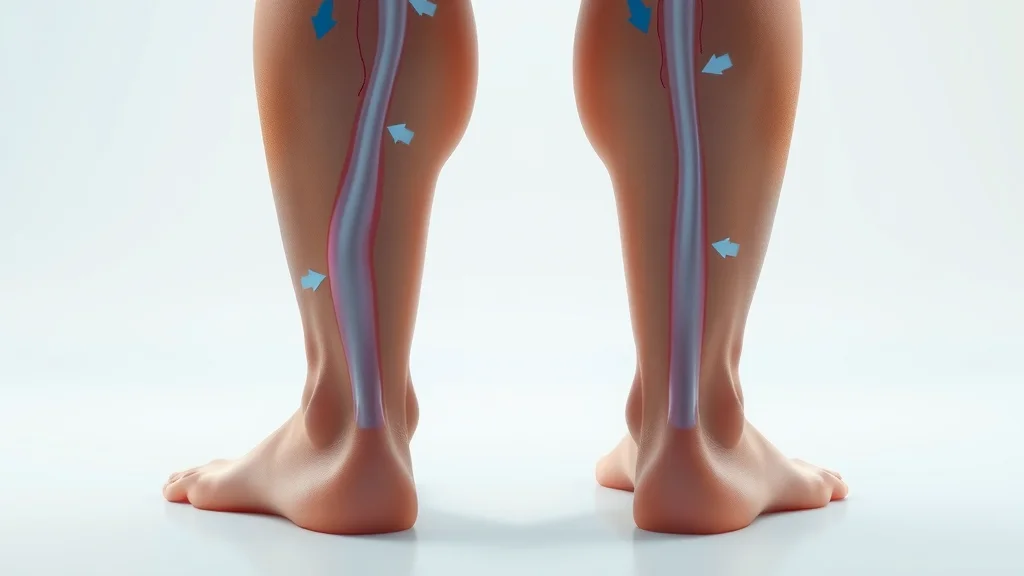
Venous Insufficiency and Swollen Ankles
Venous insufficiency is one of the most common medical reasons for swollen ankles and edema, particularly as we age. This condition occurs when valves in your lower leg veins fail to function properly, making it hard for blood to return efficiently to the heart. The resulting backup increases pressure in the veins, forcing fluid into surrounding tissue and causing swelling, especially after standing or sitting for long periods. You may also notice aching, heaviness, or skin color changes in your lower legs and ankles.
Risk factors for venous insufficiency include prolonged periods of immobility, obesity, pregnancy, and a personal or family history of varicose veins. Over time, unaddressed venous problems can progress to more severe swelling, skin ulcerations, or chronic pain. If your swollen ankle is accompanied by visible vein patterns, persistent puffiness, or changes in skin texture, it’s wise to consult a vascular specialist for thorough assessment and personalized management.
Heart Failure as a Cause of Edema
Heart failure—a condition in which the heart isn’t able to pump blood efficiently—often leads to pronounced edema in the lower legs and feet. As the heart’s pumping capacity falters, blood returning from the lower parts of your body slows down and pressure builds, resulting in excess fluid leaking into surrounding tissues. This fluid retention frequently presents as swelling in both ankles, especially after sitting for long periods or as the day progresses, and may be accompanied by symptoms like shortness of breath, rapid weight gain, or fatigue.
It’s critical to recognize these signs early. Heart failure-related edema does not resolve by simply elevating the legs and may worsen quickly without prompt medical intervention. Those with a history of high blood pressure, heart disease, or previous episodes of swelling should remain vigilant for changes in swelling or breathing, as these may signal an urgent need to adjust medications or revisit treatment plans with a healthcare provider.
Blood Clots, Swollen Ankles, and Warning Signs
While symmetrical swelling in both legs is typically linked to general fluid retention or heart failure, blood clots (known medically as deep vein thrombosis, or DVT) often cause one-sided swelling—usually in a single ankle or lower leg. Blood clots can develop after injury, surgery, periods of immobility, or for those with underlying clotting disorders. If you notice a sudden, painful swollen ankle associated with redness, warmth, or tenderness in the affected limb, seek urgent medical attention—this combination of symptoms could indicate a blocked deep vein that requires prompt treatment to prevent life-threatening complications such as pulmonary embolism.
Warning signs of a blood clot include swelling that comes on quickly, persistent pain, and sometimes a low-grade fever or visible discoloration of the skin. Although other causes like infection or trauma may cause similar symptoms, any unexplained, severe, or persistent swelling should always be evaluated by a nurse or doctor as soon as possible.
| Cause | Description | Signs/Symptoms |
|---|---|---|
| Venous Insufficiency | Poor vein valve function in legs/failure to return blood | Swelling, aching, heaviness |
| Heart Failure | Weak heart pumps blood inefficiently | Edema, shortness of breath |
| Blood Clot | Blockage in deep veins (DVT) | Swelling, pain, redness |
| Fluid Retention | Excess fluid collects in lower limbs | Puffy ankles/feet |
Recognizing and Assessing Swollen Ankles and Edema
Symptoms: When is Swelling in the Legs and Feet Abnormal?
Swelling in the legs and feet is only occasionally a simple reaction to hot weather or standing for long periods. True concern arises when swelling is sudden, persistent, or accompanied by unusual symptoms like pain, heat, redness, or changes in skin color. Abnormal swelling usually extends beyond normal, mild puffiness, and often persists despite rest or foot elevation. Warning signs prompting urgent medical attention include inability to relieve swelling overnight, difficulty breathing, or swelling localized to just one lower leg or ankle.
Additionally, pay close attention if your swollen ankle is linked with visible skin changes such as mottling, bruising, or wounds that heal slowly. If your legs may feel heavy or tight, or if you notice tender areas, persistent pain, or a sudden increase in ankle swelling, it may suggest deeper issues such as venous insufficiency, fluid retention from heart failure, or even a blood clot. Identifying these red flags early makes timely diagnosis and management possible.
How to Check Edema: Tips for Adults and Children
Checking for edema is simple but critical for early detection and assessment. In adults, use the press test: gently press your thumb into the swollen area for a few seconds, then release. If a dimple, or “pit,” remains, this is known as pitting edema, a classic sign of fluid retention. Also, observe for color or temperature differences—red, warm skin or blue-tinged extremities may point to compromised blood flow or infection. It’s also important to monitor any new pain, tenderness, or changes in sensation, including numbness or burning.
For children, be extra gentle. Note the location, pattern, and degree of swelling, and look for symptoms like fever, irritability, or delayed development. Pediatric evaluation is always recommended for persistent or unexplained swelling, as growing children may experience different causes than adults. Consistent monitoring, paired with prompt communication with a healthcare provider, helps prevent complications in all age groups.

Understanding Bruising and Skin Changes With Edema
Long-standing edema stretches the skin, making it more fragile and prone to secondary issues like bruising, color changes, or even slow-healing sores. As your skin becomes taut and thinned by persistent fluid retention, even slight bumps or pressure may leave distinct blue or brown marks. You also may see an unusual shiny “polish” to the skin and a loss of normal hair growth in the swollen area.
The risk of infection, tissue breakdown, and scarring goes up in areas of the legs and feet affected by chronic swelling. Deep bruising, wounds that leak fluid, or patches of hard, thickened skin all warrant medical review, especially for those with diabetes or impaired circulation. Monitor these changes closely and make sure to discuss them with your nurse or doctor during regular check-ups.
- Press test: gently press the swollen area to check if a dimple remains (pitting edema)
- Look for color or temperature changes
- Monitor for pain, tenderness, or sudden increase in swelling
When Swollen Ankles and Edema Require Urgent Attention
When Should I Be Concerned About Swollen Ankles?
Swollen ankles and edema usually resolve with rest or lifestyle adjustments, but urgent medical evaluation is necessary if you experience sudden swelling, intense pain, warmth, or redness—particularly if it affects only one leg. These symptoms, alongside trouble breathing or a known history of heart failure, venous insufficiency, or blood clot, could indicate a life-threatening emergency. Never ignore swelling that comes on at the same time as chest pain or severe breathlessness; call for medical help immediately.
Answer: Seek prompt care if you have sudden swelling, pain, heat, redness, trouble breathing, or history of heart failure, venous insufficiency, or blood clot.
How to Manage and Reduce Swollen Ankles and Edema
How Do You Get Rid of Edema in Your Ankles?
Reducing edema and swelling in your ankles involves a combination of daily habits and medical oversight. Start by elevating your legs above heart level for 30 minutes several times a day—this helps fluid return to your upper body. Regular, light exercise boosts blood circulation and lymphatic drainage. Wearing compression socks or stockings, if approved by your healthcare provider, supports your veins and can help minimize ankle swelling.
Limiting sodium in your diet—by reducing processed foods and avoiding added salt—can decrease water retention. Stay hydrated, as dehydration prompts your body to retain excess fluid. If you’re taking medications known to cause swelling or water retention, discuss possible adjustments with your physician. Topical skin care (e.g., gentle lotion) can also help prevent irritation or breakdown of swollen skin.
Answer: Elevate your legs, exercise regularly, wear compression socks, limit sodium, and address fluid retention. Discuss medication adjustments with your doctor.
Lifestyle Changes for Reducing Fluid Retention
Simple, consistent actions can powerfully reduce swelling and fluid retention in your lower legs and feet. Keep moving throughout the day, even with modest stretches or walking if sitting for long periods. Monitor your weight daily—sudden increases may be a sign of underlying fluid retention. Wear supportive shoes, and avoid standing or sitting for hours at a time without movement.
Eating a balanced diet with reduced salt and sugar helps control both blood pressure and fluid levels. Proper hydration maintains cellular health and improves the efficiency of your lymphatic system. Track any new or increasing swelling, and talk regularly with your care team about medication, exercise, and dietary changes to prevent complications.
- Stay active
- Limit salt intake
- Hydrate properly
- Monitor your weight and leg swelling
- Wear supportive shoes

Can Edema Cause Bruising and Other Skin Problems?
Answer: Yes, edema can stretch the skin, making it fragile and prone to bruising or slow-healing wounds.
Chronic or severe edema places ongoing pressure on the skin and blood vessels of your ankles and lower legs. This tension makes the skin more delicate, increasing the risk of easy bruising from minor bumps or friction. Over time, the skin may become wrinkled, shiny, or even discolored (bluish or brown) as a result of persistent swelling. Wounds may develop or heal more slowly, particularly in older adults or those with diabetes or vein problems.
If you notice frequent bruises, open sores, or dark patches on your swollen ankle or lower leg, it’s essential to protect the skin and seek guidance from your healthcare team. Addressing fluid retention early, wearing protective footwear, and moisturizing dry skin can all help prevent these secondary complications.

How to Check Edema in Children: Special Considerations
Answer: Use gentle pressure to check for pitting, note swelling patterns, and be alert to accompanying symptoms. Pediatric assessment is essential.
Swelling and edema in children are less common than in adults but should always be evaluated promptly. Use gentle finger pressure to check if a visible dimple remains after releasing, which may indicate fluid retention. Observe the swelling for symmetry, color changes, or any temperature differences. Children with swollen ankles or legs should also be checked for fever, pain, sudden irritability, or difficulty walking.
Pediatric edema may be linked to infections, allergic reactions, or rare immune or kidney disorders. Never delay medical evaluation if swelling appears suddenly, worsens quickly, or is accompanied by systemic symptoms (such as rash or respiratory distress). Establishing the underlying cause and intervening early maximizes the chance for a full recovery in children.

Educational video overview explaining swollen ankles and edema, causes, and early signs.
Watch:Step-by-step self-care and prevention tips for swollen ankles and edema.
Watch:Frequently Asked Questions on Swollen Ankles and Edema
-
What are the top causes of swollen ankles and edema?
Venous insufficiency, heart failure, fluid retention from a high salt diet or medication, long periods of standing or sitting, blood clots, and certain medical conditions affecting the kidneys or lymphatic system are all frequent causes. -
Can diet and hydration make a difference?
Absolutely. Reducing salt in your diet, staying well-hydrated, and eating balanced whole foods can all help decrease water retention and reduce swelling in your legs and ankles. -
Are swollen ankles always a sign of heart failure?
No. While heart failure is a major cause, swelling can also stem from vein problems, high salt intake, inactivity, reactions to heat, or medications. See your doctor for unexplained or persistent swelling. -
What medications can worsen or improve edema?
Certain blood pressure drugs, steroids, hormone therapies, and diabetes medicines can cause or worsen edema. Diuretics (water pills) may help reduce swelling but should only be used under medical supervision. -
Is swelling in one ankle more dangerous than both?
Yes – sudden, unexplained swelling in only one lower leg or ankle, especially with pain or color change, should be evaluated urgently for blood clot or localized infection.
Expert Insights: Quotes on Swollen Ankles and Edema
"Early recognition of swelling in the legs and feet can dramatically change the outcome for conditions like venous insufficiency and heart failure." – Dr. Thomas Lin, Vascular Specialist
"Simple daily prevention can reduce fluid retention, support healthy circulation, and prevent dangerous complications." – Dr. Anjali Desai, Internist
Key Takeaways About Swollen Ankles and Edema
- Know the difference between minor swelling and signs of critical illness
- Track changes in your legs and feet regularly
- Address fluid retention and swollen ankles early
- Consult your doctor for persistent or unexplained edema
Your Next Steps: Promote Longevity and Circulation
Discover daily habits backed by both Mediterranean tradition and modern research — download the 5 Daily Rituals for Longevity.
Conclusion: By understanding swollen ankles and edema, monitoring your symptoms, and adopting simple habits, you can protect your circulation, mobility, and overall health—starting today.
If you’re eager to expand your knowledge beyond personal health and explore how community-wide initiatives can impact well-being, consider reading about the EPA’s campaign to reduce problem waste and protect communities. This broader perspective highlights how environmental health and proactive public measures can support healthier living for everyone, offering valuable insights for those committed to long-term wellness.
 Add Row
Add Row  Add
Add 




Write A Comment